August 2019 | Point of View
The new business model for health plans: Delivering a member-centric omnichannel experience
A health plan’s success depends on its ability to evolve and modernize to meet new expectations. This begins with the adoption of a member-centric, omnichannel business model.
- The business model for health plans is rapidly evolving. To meet new expectations around the delivery of holistic member experiences, health plans must provide personalized, information-rich services in a consistent, coordinated manner across members’ preferred communication channels. Doing so means embracing a member-centric, omnichannel ethos wherein member experience is seen as the product and the organization offers choice, transparency, and simplified, self-service interactions.
- Health plans are uniquely positioned to be industry leaders in consumer engagement. Adopting new processes and technologies for leveraging the wealth of member health information at their disposal will yield substantial rewards in terms of cost savings, member satisfaction, and opportunities for expanded capabilities. A digital communications architecture that prioritizes seamlessness and flexibility is the way to get there.
- Achievement of a member-centric, omnichannel operating model is not without its challenges. Siloed operations, fragmented technology, and disparate communications are common characteristics that many health plans must overcome in order to move from single-channel, back-and-forth communications to the kinds of integrated experiences that consumers have come to expect. This requires a culture change, and it’s best to start small, work iteratively, and maintain constant alignment to a strong vision.
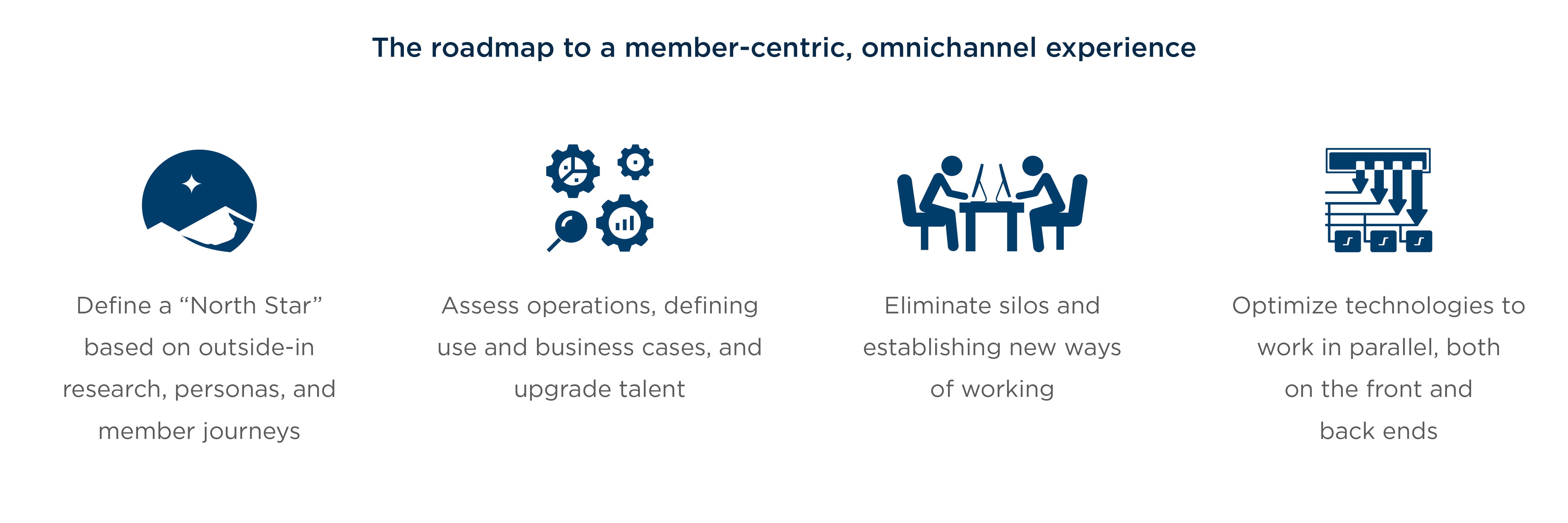
- The roadmap to success covers four key areas. The health plan must define and communicate its desired outcome across the organization, assess operations and align talent appropriately, eliminate silos and establish new ways of working, and optimize technology to support a member-focused operating model. Taking a phased approach structured around a portfolio of steps needed to achieve a minimum viable product will allow for the development of the skills, experience, and momentum needed for change on an enterprise-wide scale.
Introduction
It’s no secret that the business model for health plans is rapidly evolving. In the past, plans were in the business of administration—maintaining provider networks and processing claims and reimbursements.
These days, they are expected to deliver a holistic experience for healthcare consumers, making use of their unique position as one of the few points in the healthcare ecosystem that has a 360-degree view of each member. This means taking on relationship advisor and care coordinator roles, helping members stay healthy, and paving the way for access to better care—roles that have historically fallen on providers or, frankly, the members themselves.
In the new order, a health plan’s success depends on its ability to evolve and modernize to meet these new expectations.2 In particular, delivering personalized, information-rich services and embracing the potential presented by new, digital technologies to engage members in a consistent, coordinated fashion across the communication platforms they prefer.
In other words, it means adopting a member-centric, omnichannel ethos—a sizeable change for most health plans as they operate today. This white paper summarizes the challenges that health plans face in this regard and describes steps they can take to overcome them.
Chapter 1: Health plans have a clear opportunity to lead the industry in consumer engagement
Companies in technology, finance, and other sectors that have taken a consumer-centric, omnichannel approach have reaped enormous benefits for their stakeholders, fueling rising expectations among consumers to the point where a holistic experience is becoming table stakes. Health plans can capitalize on the lessons these trailblazing industries have learned and the methods they have pioneered in order to deliver better services at lower costs for themselves and their members.
The potential rewards are substantial. Already, digitally mature health plans provide members with secure omnichannel media—portals, websites, mobile apps, and the like—providing multiple, synchronized views of up-to-date information on members’ medical history. This seamlessness and flexibility offers numerous benefits to the overall member experience, including choice, transparency, simplified interactions, and the ability to self-serve, all with the intent to lead to a healthier population.
A member-centric framework can set the stage for machine learning and predictive analytics—capabilities that will cut costs, increase productivity, and drive down adverse health events. ”
For the enterprise, embracing the omnichannel imperative enhances visibility into plan performance as measured through factors such as customer feedback and improved member health outcomes and helps managers identify data gaps that inhibit a tailored, integrated member experience. This member-centric framework can result in reductions in call-center costs, inbound paper vendor processing, and outbound print correspondence. It can also set the stage for further technical and operational advancements.
Many health plans, however, have a long way to go before they can shift toward an omnichannel, member- centric approach.
Chapter 2: Health plans are entrenched in structures that inhibit an omnichannel experience
In our 10-plus years of experience advising health plans in the member communication and marketing space, we have observed that while many grasp the potential of the omnichannel imperative, their culture and business processes frequently pose obstacles to achieving that potential. Obstacles include:
Collectively, cultural norms establish health plans as single-channel, back-and-forth communicators that prevent them from delivering a smooth, holistic experience for their members. ”
Collectively, cultural norms like these establish health plans as single-channel, back-and-forth communicators that prevent them from delivering a smooth, holistic experience for their members. The good news is that the experience of tech pioneers like Amazon and Netflix along with that of legacy leaders like JP Morgan Chase has created a wealth of knowledge about how organizations can transition from limited, traditional operations into a more dynamic, digital approach like that of the omnichannel imperative.
Chapter 3: A roadmap to overcome those challenges covers 4 key areas
To achieve the customer-focused, omnichannel experience that consumers have come to expect— personalized, seamless, immediate, and information- rich—health plans need to integrate data, technology, content, and communications. They must overhaul and update their processes to become more agile. And they must deliver more customized, timely, and relevant content that addresses health needs in addition to transactions through multiple communication channels, giving members choices in how they wish to interact with the organization. But how? And where does an organization start?
Most broadly, achieving the omnichannel imperative requires a culture change focused on bringing people together in a more cohesive way that mirrors the desired member experience. More specifically, it requires reorienting the health plan to knock down process and technology silos in favor of cloud applications and agile, multidisciplinary teams. This will pave the way for scaling digital capabilities and optimizing processes so that each business function in the organization is committed to the same member experience, not just marketing and communications.
1. Define a north star
As a first step, health plan leadership should define the outcome it seeks for the organization, or its North Star. Leadership needs to be able to articulate how the organization will harness the power of digital communications within an omnichannel architecture to differentiate the enterprise as a member-focused plan. A clearly defined North Star enables the organization to envision the journey required to achieve this goal.
Defining a North Star requires the health plan to conduct research on its member base to gain a more intimate understanding of the key touchpoints, pain points, and breakdowns in various member journeys. This research should include interviews, surveys, persona building, and journey mapping. It should emphasize an outside- in perspective and involve a Net Promoter Score (NPS) program that can pinpoint priorities capable of delivering the most impact per dollar spent.
In addition, this research will help build the internal messaging necessary to support an effective culture shift and obtain buy-in across the enterprise. Employees who understand and share the organization’s vision of its ideal member strategy will be far more likely to go the extra mile to help make that vision a reality. Simply put, an organization cannot reach its desired destination unless all stakeholders know exactly what that destination is.
Once the North Star is identified and communicated, the health plan can begin making key operational changes to overcome obstacles and map out a portfolio of steps needed to achieve its goals and reach a minimum viable product.
Further Reading
2. Assessing operations and aligning the right talent
Upgrading the organization’s skills and talent to meet the omnichannel imperative means instilling a member-centric ethos built around professionals with the ability to discern customer needs and get creative about crafting experiences on digital and traditional channels—and people who think end-to-end and understand how to operate in an agile environment, and are comfortable helping people change.
As a first step, the organization must assess the current state of operations and understand the roles and responsibilities involved. The member journey maps produced during the previous phase will help elucidate the current member experience and identify “make it or break it” moments in an ideal future state.
3. Eliminate silos to establish new ways of working
Health plans are typically compartmentalized into silos, or functional towers of responsibility. This, of course, is not unusual. Most legacy companies are organized this way. The challenge is that silos tend to prioritize departmental goals rather than the overall organization’s objectives, and employees within silos see only a fragmented view of the member experience. This fragmentation prevents health plans from delivering a holistic, member- centric experience and makes the organization appear bureaucratic and disconnected.
Health plans of the future upend this approach. In place of product development, marketing, claims, service, finance, provider network management, and the like, the member is the central organizing principal. Employees, processes, and incentives are organized around goals such as member onboarding, member services, and clinical pathways.
Health plans should structure themselves more like agile digital companies, always adapting and improving, where cross-functional teams cooperate to achieve clearly envisioned goals and the experience is seen as the product. ”
With the North Star established and any talent gaps addressed, a data-driven, member-centric approach can be leveraged to define an end-to-end operating model. In such a model, member experiences are owned by each line of business and multiple teams touch a portion of each process, minimizing handoffs, and providing clear accountability. Workflows are optimized for efficiency and tracked for continuous improvement against the overall objective of serving members’ needs rather than merely processing their transactions.
Employees will need to understand that under the new model, there will be many changes to the way they work, the processes they use, and how they collaborate. These new multidisciplinary, agile pods will be staffed according to member needs—for instance, by specialists in business, process, customer experience, technology, and data—forming integrated customer-focused teams that build specific capabilities and think end-to-end.

Finally, to ensure that the new way of working reflects the North Star, employee incentives will need to be aligned with the goals of the transformation. Leaders can empower employees by clearly defining KPIs—many of which may be borrowed from other industries that have more experience with these concepts—that stress the importance of member-centric behavior. These KPIs should be formalized and publicized throughout the organization in order to ensure awareness of the project’s status and remind employees of the objectives.
4. Optimize technology to deliver a member-focused operating model
The ever-evolving, member-focused business model also demands that health plans capitalize on the wealth of data they collect. Plans have a unique view of their members’ medical records that may otherwise be scattered across labs, hospitals, and doctors’ offices.
Once health plans begin the transformation journey and establish agile, cross-functional teams, the collective data can be aggregated across the board to truly change the way an organization interacts with its members. Insights can be developed and sharpened once capabilities are enabled to capture data from members via web, text, email, phone, and social media. These insights can ultimately assist in coordinating care, promoting healthy lifestyles, and developing best practices and policies for the broader community of members.
By putting organized data and associated insights in the hands of the teams responsible for engaging members, a true relationship can develop between the health plan and its members.
”
If properly leveraged, data can signal where members are in a particular care journey, providing a sense of understanding and intimacy with the membership base.
Managers can make use of dashboards and reports, such as those available from issue-resolution platforms, to gain a deeper understanding of the health plan’s operational pain points, particularly any gaps or inconsistencies in the member experience. Predictive analytics can then help inform member communications and support efficient issue identification and resolution.
With this knowledge, proactive outreach can occur to ensure the member is prepared and comfortable for whatever comes next. Customer service representatives, with access to an integrated customer- relationship-management platform paired with next- best-action analytics, will have useful insights into what a member is likely to be calling about based on their previous interactions with the plan, regardless of the interaction channel.
When embarking upon a digital transformation, it is important to avoid efforts that are too large to handle at once. Ideally, two or three use cases will be defined up front along with the underlying technology required to support them. Once the prioritized capabilities are available to the new agile and cross-functional teams, the health plan can go a long way toward realizing the omnichannel, member-focused imperative.
Ultimately, the proactive use of data will not only advance learning and improve member relations, it will promote better health based on the information we know about each individual. Better service will help catalyze superior medical outcomes, benefitting both the plan and its members.
Conclusion
Next Steps
Optimizing technology will better position health plans to meet evolving customer expectations, as most members have grown accustomed to interacting with companies through multiple digital channels (e.g., apps, portals, and social media). Moreover, digital channels pair well with multi-source data capture and aggregation, providing visibility into how members traverse their healthcare journeys and interact with the health plan, whether through print ads, navigating a member portal, phoning the call center, or responding to a health and wellness survey. The omnichannel imperative requires that member experiences be consistent and seamless across each of these avenues.
In our experience, the best approach to addressing the member-focused, omnichannel imperative is to clearly define the North Star and create a broad vision for transformation. Implementation can begin with two or three member-oriented use cases that enable true customer intimacy while bringing cost or revenue benefits to the organization. Beginning with an enterprise approach to transformation is inadvisable due to the complexity and technical depth required at that scale, particularly because of the broader process changes involved—changes that are insurmountable in a short period of time.
Once the health plan has sufficiently analyzed its operational landscape, a backlog of customer priorities can be created and appropriately skilled, cross-functional teams can develop proofs of concept. Taking this phase- driven, gradual approach will allow for the development of the skills, experience, and organizational momentum needed to take on bigger tasks, and eventually roll out the transformation across the enterprise.